David Metcalf’s last act in life was an attempt to send a message — that years as a Navy SEAL had left his brain so damaged that he could barely recognize himself.
He died by suicide in his garage in North Carolina in 2019, after nearly 20 years in the Navy. But just before he died, he arranged a stack of books about brain injury by his side, and taped a note to the door that read, in part, “Gaps in memory, failing recognition, mood swings, headaches, impulsiveness, fatigue, anxiety, and paranoia were not who I was, but have become who I am. Each is worsening.”
Then he shot himself in the heart, preserving his brain to be analyzed by a state-of-the-art Defense Department laboratory in Maryland.
The lab found an unusual pattern of damage seen only in people exposed repeatedly to blast waves.
The vast majority of blast exposure for Navy SEALs comes from firing their own weapons, not from enemy action. The damage pattern suggested that years of training intended to make SEALs exceptional was leaving some barely able to function.
But the message Lieutenant Metcalf sent never got through to the Navy. No one at the lab told the SEAL leadership what the analysis had found, and the leadership never asked.
It was not the first time, or the last. At least a dozen Navy SEALs have died by suicide in the last 10 years, either while in the military or shortly after leaving. A grass-roots effort by grieving families delivered eight of their brains to the lab, an investigation by The New York Times has found. And after careful analysis, researchers discovered blast damage in every single one.
It is a stunning pattern with important implications for how SEALs train and fight. But privacy guidelines at the lab and poor communication in the military bureaucracy kept the test results hidden. Five years after Lieutenant Metcalf’s death, Navy leaders still did not know.
Until The Times told the Navy of the lab’s findings about the SEALs who died by suicide, the Navy had not been informed, the service confirmed in a statement.
A Navy officer close to the SEAL leadership expressed audible shock, and then frustration, when told about the findings by The Times. “That’s the problem,” said the officer, who asked not to be named in order to discuss a sensitive topic. “We are trying to understand this issue, but so often the information never reaches us.”
The lack of communication has led Navy leaders to overlook a potentially critical threat to its elite special operators. When the commander of SEAL Team 1 died by suicide in 2022, SEAL leaders responded by ceasing nearly all operations for a day so the force could learn about suicide prevention. According to four people with knowledge of the commander’s case, his brain was later found to have extensive blast damage, but because the leaders were not told, they never discussed the threat of blast exposure with the force.
Evidence suggests that the damage may be just as widespread in SEALs who are still alive. A Harvard study, published this spring, scanned the brains of 30 career Special Operators and found altered brain structure and compromised brain function in nearly all of them. The more blast exposure the men had experienced, the more problems they reported with health and quality of life.
That study was funded by Special Operations Command, which has been at the forefront in the military’s effort to understand the issue. In December, the study’s main author briefed the command’s top leaders, including from the Navy SEALs.
“We have a moral obligation to protect the cognitive health and combat effectiveness of our teammates,” Rear Adm. Keith Davids, the commander of Navy Special Warfare, which includes the SEALs, said in a statement. He said the Navy is trying to limit brain injuries “by limiting blast exposure, and is actively participating in medical research designed to enhance understanding in this critical field.”
But without the data on suicides, a key piece of the problem was never discussed at the briefing.
Blows to the Head
The communication breakdown is part of a broader disconnect in the Defense Department, which spends nearly $1 billion each year on brain injury research, and many billions more to train and equip troops, but does comparatively little to ensure that the latest science on brain injury informs practices in the ranks.
Lieutenant Metcalf’s wife, Jamie Metcalf, said in an interview that she had come to see his death as a an effort to draw attention to a widespread problem.
“He left an intentional message, because he knew things had to change,” she said. When told the information about his brain had not reached the SEAL leadership, she sighed and said, “You’re kidding me.”
The military readily acknowledges that traumatic brain injury is the most common injury from recent conflicts. But it is struggling to understand how many of those injuries are inflicted by the shock waves unleashed by troops’ own triggers.
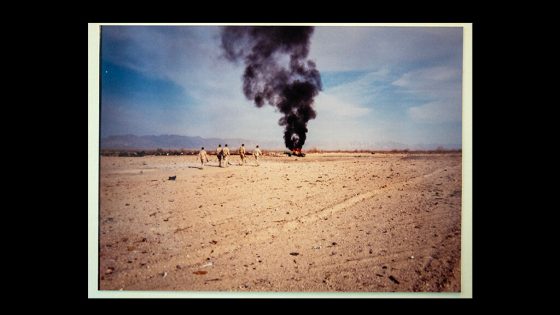
There are signs that the damage can come from a wide array of weapons. Artillery crew members who fired thousands of rounds in combat came home plagued by hallucinations and psychosis. Mortar teams suffered from headaches and deteriorating memory. Reliable soldiers suddenly turned violent and murdered neighbors after years of working around the blasts from tanks and grenades in combat or in training.
Blast waves may kill brain cells without causing any immediately noticeable symptoms, according to Dr. Daniel Daneshvar, chief of brain injury rehabilitation at Harvard Medical School.
“People may be getting injured without even realizing it,” Dr. Daneshvar said. “But over time, it can add up.”
People’s brains can often compensate until injuries accumulate to a critical level, he said; then, “people kind of fall off a cliff.”
In many cases, doctors treating the injured troops give them diagnoses of psychiatric disorders that miss the underlying physical damage. Much of what is categorized as post-traumatic stress disorder may actually be caused by repeated exposure to blasts.
The stories of the SEALs who died by suicide point to a troubling pattern in the elite force.
Their average age was 43. Each had deployed to combat a number of times, but none had been wounded by enemy fire. All had spent years firing a wide arsenal of powerful weapons, jumping from airplanes, blowing open doors with explosives, diving deep underwater and learning to fight hand to hand.
Over the years they had developed the expertise and sharp judgment of seasoned special operators. But late in their careers, the effects of years of repeated blast exposure ate those skills away.
Around the age of 40, nearly all of them started to struggle with insomnia and headaches, memory and coordination problems, depression, confusion and, sometimes, rage.
“The first thing people think is, it must be PTSD, but that never made sense to me — it didn’t fit,” said Jennifer Collins, whose husband, retired Chief Petty Officer David Collins, was a SEAL for 20 years and died in 2014, just over a year after leaving the Navy.
A Late-Career Breakdown
Ms. Collins is the reason that the brains of a high proportion of the SEALs who died by suicide made it to the Defense Department’s lab.
Her husband was in many ways a typical SEAL: smart, confident, easygoing and high-achieving. He deployed to Afghanistan twice and to Iraq three times. When he was not deployed, he was away from home for hundreds of days each year in training.
Combat never seemed to faze Mr. Collins, but near the end of his Navy career, he started to change in subtle ways that Ms. Collins pieced together only in retrospect. He began to avoid social gatherings. He struggled to sleep. He started to make strange, obsessive family schedules and become irritated when they were not followed. Some simple chores, like raking leaves into a tarp, started to confound him. He would step out the door to go to work, realize that he had forgotten his keys, go back inside to get them and then forget why he had returned.
All were signs of brain injury. But at the time, the military generally associated brain injury with big blasts from roadside bombs — something Mr. Collins never experienced. No one was telling the troops that repeated exposure to routine blasts from their own weapons might be a risk.
Mr. Collins’s mental health took a sudden plunge when he was 45. He had left the Navy and started a civilian job teaching troops to operate small drones. One morning, well before the sun was up, he called his wife in a panic from a work trip, saying he had forgotten how to do his job and had not slept in four days.
“He was super anxious, almost paranoid,” Ms. Collins recalled. “He was nothing like my husband.”
When Mr. Collins returned to the couple’s home in Virginia Beach, doctors scanned his brain with magnetic resonance imaging but found nothing abnormal. They eventually gave him a diagnosis of depression, anxiety and post-traumatic stress disorder, and prescribed a number of drugs for sleep and mood. They didn’t help.
He then went to a specialty clinic for brain injury but failed to find relief.
Everyday tasks like booking a flight became so arduous that he would puzzle over them for hours. He was sleepless and agitated — scared that his mind was slipping away.
In March 2014, three months after placing the frantic pre-dawn call to his wife, he went to return a few library books, dropped off a tuition check at his son’s kindergarten, and then drove to a secluded side street. He sent a text to his wife saying, “So sorry, baby. I love you all,” and ended his life.
“I knew, with all he had been going through, that the text could only mean one thing,” Ms. Collins said.
When the police came to the house to confirm his death, she was adrift in grief and confusion. But one determined thought floated to the front of her mind.
“I told the police — I was adamant — that I wanted his brain donated to research,” she recalled. “I wanted to try to find some answers.”
Visible Under a Microscope
In Bethesda, Md., the Defense Department had built a lab in 2012 called the Department of Defense Brain Tissue Repository, whose goal was to gather the brains of deceased veterans to look for clues to the two most widespread injuries of recent wars, PTSD and traumatic brain injury. But two years after opening, the lab faced a fundamental problem: It had no brains to study.
The lab depended on tissue donations from the families of war veterans who had recently died, but few families knew it existed, and the lab’s bylaws barred it from cold-calling grieving families to ask. Brain tissue deteriorates quickly; by the time most families found out about the lab, it was too late.
Ms. Collins’s quick decision meant that her husband’s brain was soon packed in ice and on its way.
That single brain revealed a pattern of damage that the head of the lab, Dr. Daniel Perl, who had spent a career studying neuropathology in civilians, had never seen before. Nearly everywhere that tissues of different density or stiffness met, there was a border of scar tissue — a shoreline of damage that seemed to have been caused by the repeated crash of blast waves.
It was not chronic traumatic encephalopathy, or C.T.E., which is found in football players and other athletes who have been repeatedly hit in the head. It was something new.
The lab’s research team started looking for similar damage in other brains. In civilians’ brains, they did not find it. Nor was it in the brains of veterans who had been exposed to a single powerful explosion like a roadside bomb. But in veterans exposed repeatedly to blasts, they found it again and again.
The team published a landmark study in 2016 reporting the pattern of microscopic damage, which they called interface astroglial scarring.
“For the first time, we could actually see the injury,” Dr. Perl said in an interview. “If you know what the problem is, you can start to design solutions.”
Dr. Perl said privacy rules bar him from discussing specific cases, but members of the families who provided brains to study say the lab found interface astroglial scarring in six of the eight SEALs who died by suicide. The other two SEALs, including Lieutenant Metcalf, had a different type of damage in the same blast-affected areas. Star-shaped helper cells called astrocytes in their brains appeared to have been repeatedly injured and had grown into gargantuan, tangled masses that barely functioned. The lab plans to publish findings on the astrocyte injuries soon.
Recent studies suggest that damage is caused when energy waves surging through the brain bounce off tissue boundaries like an echo, and for a few fractions of a millisecond, create a vacuum that causes nearby liquid in the brain to explode into bubbles of vapor. Those tiny explosions are violent enough to blow brain cells apart in a process known as cavitation.
Dr. Perl shared with Ms. Collins what he had found in her husband’s brain in 2016, and she made it her mission to get more families to donate.
Spreading the Word
For the next several years, Ms. Collins told anyone who would listen about his case — Navy SEAL leaders, veterans’ groups, gatherings of wives. And when a career SEAL died by suicide, a call from Ms. Collins often soon followed. In 2017, she called the parents of Special Operator First Class Ryan Larkin. A few months later, she sat down with the wife of retired Chief Petty Officer Bill Mulder.
“She had the paperwork in her hand, and said, ‘I think this would be a smart thing to do,’” Mr. Mulder’s wife, Sydney Mulder, recalled in an interview. “I was in a blur, but I didn’t hesitate, and I’m glad I did it.”
Ms. Collins’s influence spread until brain donation became somewhat common for Special Operations troops. But little of what the researchers have learned from those brains made it back to the SEAL team leadership.
Mr. Mulder, like Mr. Collins, had spent a career in the SEALs but had never been wounded. He was an explosives expert in the elite SEAL Team 6, exposed to thousands of blasts in training.
After years of steady service, he went into a steep decline. He couldn’t sleep and was constantly misplacing things. Frustration would send him into a rage. He stewed over negative interactions in his squadron and started drinking before work.
“For all the years I’d known him, he had been such a capable man,” Ms. Mulder said. “He would wake up at six in the morning and get his workout. He was incredibly smart and organized and diligent. And then he just wasn’t.”
After years of trying to get help from doctors who largely overlooked the possibility of brain injury, Mr. Mulder took his own life at age 46.
Jamie Metcalf also noticed a sudden decline in her husband when he returned in 2018 from his fifth deployment. For years, Lieutenant Metcalf had been a high achiever. He was an enlisted SEAL sniper, and taught martial arts to other SEALs. A few years before he died, he decided to pursue a military medical career, became an officer and sailed through the demanding training program for physician assistants.
But after his final deployment, he was moody, confused and plagued by headaches. He put wet laundry in the dryer on top of dry clothes. One day he emptied out the kitchen cupboards to organize them, then left everything in piles on the counter.
“It was so unlike him — he had always been so organized,” Ms. Metcalf said. “Now I know he was afraid there was something happening in his brain, but at the time, I think he tried to hide it.”
He died a few months later at age 42.
The men who died by suicide represent only a small fraction of the career SEALs with signs of brain injuries after years around blasts.
Several SEAL veterans said in interviews that many of their former teammates are now divorced and grappling with depression, paranoia and substance abuse — all of which can be caused by deteriorating brain function. Desperate calls from suicidal friends are common, they said.
Ms. Metcalf saw how broad the problem was when she read the letter her husband had left about his brain injury symptoms to two of his SEAL friends.
“One of them was crying on my lap, saying, ‘That’s me, that’s me,’” she said. “And the other told me a lot of them have problems, but don’t know what to do.”
If you are having thoughts of suicide, call or text 988 to reach the 988 Suicide and Crisis Lifeline or go to SpeakingOfSuicide.com/resources for a list of additional resources.
Source Agencies