Ziyad Al-Aly is chief of research and development at VA St. Louis Health Care System and a clinical epidemiologist at Washington University in St. Louis.
Since 2020, the condition known as long COVID-19 has become a widespread disability affecting the health and quality of life of millions of people across the globe and costing economies billions of dollars in reduced productivity of employees and an overall drop in the work force.
The intense scientific effort that long COVID sparked has resulted in more than 24,000 scientific publications, making it the most researched health condition in any four years of recorded human history.
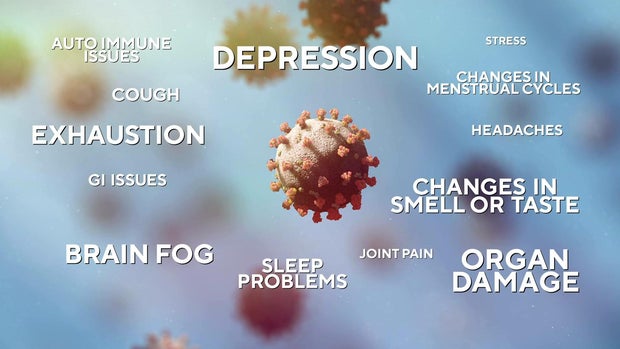
Long COVID is a term that describes the constellation of long-term health effects caused by infection with the SARS-CoV-2 virus. These range from persistent respiratory symptoms, such as shortness of breath, to debilitating fatigue or brain fog that limits people’s ability to work, and conditions such as heart failure and diabetes, which are known to last a lifetime.
I am a physician scientist, and I have been deeply immersed in studying long COVID since the early days of the pandemic. I have testified before the U.S. Senate as an expert witness on long COVID, have published extensively on it and was named as one of Time’s 100 most influential people in health in 2024 for my research in this area.
Over the first half of 2024, a flurry of reports and scientific papers on long COVID added clarity to this complex condition. These include, in particular, insights into how COVID-19 can still wreak havoc in many organs years after the initial viral infection, as well as emerging evidence on viral persistence and immune dysfunction that last for months or years after initial infection.
How long COVID affects the body
A new study that my colleagues and I published in the New England Journal of Medicine on July 17, 2024, shows that the risk of long COVID declined over the course of the pandemic. In 2020, when the ancestral strain of SARS-CoV-2 was dominant and vaccines were not available, about 10.4% of adults who got COVID-19 developed long COVID. By early 2022, when the omicron family of variants predominated, that rate declined to 7.7% among unvaccinated adults and 3.5% of vaccinated adults. In other words, unvaccinated people were more than twice as likely to develop long COVID.
While researchers like me do not yet have concrete numbers for the current rate in mid-2024 due to the time it takes for long COVID cases to be reflected in the data, the flow of new patients into long COVID clinics has been on par with 2022.
We found that the decline was the result of two key drivers: availability of vaccines and changes in the characteristics of the virus — which made the virus less prone to cause severe acute infections and may have reduced its ability to persist in the human body long enough to cause chronic disease.
Despite the decline in risk of developing long COVID, even a 3.5% risk is substantial. New and repeat COVID-19 infections translate into millions of new long COVID cases that add to an already staggering number of people suffering from this condition.
Estimates for the first year of the pandemic suggests that at least 65 million people globally have had long COVID. Along with a group of other leading scientists, my team will soon publish updated estimates of the global burden of long COVID and its impact on the global economy through 2023.
In addition, a major new report by the National Academies of Sciences Engineering and Medicine details all the health effects that constitute long COVID. The report was commissioned by the Social Security Administration to understand the implications of long COVID on its disability benefits.
CBS2
It concludes that long COVID is a complex chronic condition that can result in more than 200 health effects across multiple body systems. These include new onset or worsening:
- heart disease
- neurologic problems such as cognitive impairment, strokes and dysautonomia. This is a category of disorders that affect the body’s autonomic nervous system — nerves that regulate most of the body’s vital mechanisms such as blood pressure, heart rate and temperature.
- post-exertional malaise, a state of severe exhaustion that may happen after even minor activity — often leaving the patient unable to function for hours, days or weeks
- gastrointestinal disorders
- kidney disease
- metabolic disorders such as diabetes and hyperlipidemia, or a rise in bad cholesterol
- immune dysfunction
Long COVID can affect people across the lifespan from children to older adults and across race and ethnicity and baseline health status. Importantly, more than 90% of people with long COVID had mild COVID-19 infections.
The National Academies report also concluded that long COVID can result in the inability to return to work or school; poor quality of life; diminished ability to perform activities of daily living; and decreased physical and cognitive function for months or years after the initial infection.
The report points out that many health effects of long COVID, such as post-exertional malaise and chronic fatigue, cognitive impairment and autonomic dysfunction, are not currently captured in the Social Security Administration’s Listing of Impairments, yet may significantly affect an individual’s ability to participate in work or school.
A long road ahead
What’s more, health problems resulting from COVID-19 can last years after the initial infection.
A large study published in early 2024 showed that even people who had a mild SARS-CoV-2 infection still experienced new health problems related to COVID-19 in the third year after the initial infection.
Such findings parallel other research showing that the virus persists in various organ systems for months or years after COVID-19 infection. And research is showing that immune responses to the infection are still evident two to three years after a mild infection. Together, these studies may explain why a SARS-CoV-2 infection years ago could still cause new health problems long after the initial infection.
Important progress is also being made in understanding the pathways by which long COVID wreaks havoc on the body. Two preliminary studies from the U.S. and the Netherlands show that when researchers transfer auto-antibodies – antibodies generated by a person’s immune system that are directed at their own tissues and organs – from people with long COVID into healthy mice, the animals start to experience long COVID-like symptoms such as muscle weakness and poor balance.
These studies suggest that an abnormal immune response thought to be responsible for the generation of these auto-antibodies may underlie long COVID and that removing these auto-antibodies may hold promise as potential treatments.
An ongoing threat
Despite overwhelming evidence of the wide-ranging risks of COVID-19, a great deal of messaging suggests that it is no longer a threat to the public. Although there is no empirical evidence to back this up, this misinformation has permeated the public narrative.
The data, however, tells a different story.
COVID-19 infections continue to outnumber flu cases and lead to more hospitalization and death than the flu. COVID-19 also leads to more serious long-term health problems. Trivializing COVID-19 as an inconsequential cold or equating it with the flu does not align with reality.
This article is republished from The Conversation under a Creative Commons license.
Source Agencies